Part I
The envelope arrived on a Wednesday afternoon, sunlight spilling across my kitchen counter.
Heavy, expensive paper. My sister’s taste.
Gold foil on white linen.
I didn’t even have to open it to know what it was.
Inside, embossed letters announced:
“Celebrate Lauren Mitchell’s Promotion to Senior Partner – Saturday, August 12th, 2:00 PM, Stonemont Country Club.”
For a second, I stared at the date, my breath catching.
August 12th.
The same day as my cranio-cervical fusion surgery.
The date I’d been waiting eighteen months for.
I set the invitation down carefully beside my hospital paperwork — the surgical consent forms, the anesthesiology briefing, and the pre-op checklist I’d read so many times I could recite it by heart.
No food or drink after midnight. Bring cervical collar. Arrange for post-op assistance.
My phone buzzed.
Mom.
“You’ll have to reschedule.”
She didn’t even say hello.
Just that. Sharp. Final.
“Mom,” I said slowly, “I’ve been waiting a year and a half for this. Dr. Henderson only operates one Saturday a month. The next available date is in February.”
“Well,” she said, her voice clipped, “Lauren’s been working toward this partnership for eight years. The party’s important. Family needs to be there.”
“I’m getting surgery to keep my head from slipping off my spine.”
“Casey,” she sighed, “you’ve been fine for months. You can wait a little longer.”
“I’m not fine.” My throat tightened. “Mom, it’s degenerative. Every month I wait, it gets worse.”
“You’ve waited this long,” she said. “What’s another six months?”
She said it like she was asking me to postpone a dentist appointment.
Like my skull wasn’t literally sliding off my spine.
Like my neck brace was just an accessory.
“And honestly,” she added, “are you sure this surgery is even necessary? Those doctors at the university hospital said you were fine.”
“Those doctors dismissed me for three years,” I whispered. “Dr. Henderson at Mayo says if I don’t get the fusion, I could become paralyzed. Or worse.”
Silence. Then:
“That seems dramatic, Casey. You’ve been saying you’re dying for years now.”
I pressed the phone tighter to my ear, trying not to cry.
“As if I want this,” I said. “As if I want to be told my skull’s detaching from my spine.”
Mom’s tone softened just enough to twist the knife. “Honey, I think sometimes you get carried away. You have to admit, every time something big happens for Lauren, you have one of your… medical episodes.”
“I’m having the surgery,” I said quietly.
“Well,” she said, “don’t expect family photos then. We’re not rescheduling two hundred guests because you chose to have your little procedure on Lauren’s day.”
And then she hung up.
The Empty Apartment
I sat there for a long time, phone still in my hand, looking at my fingers.
They bent backward at impossible angles — a hallmark of Ehlers-Danlos syndrome.
My skin stretched like taffy. My joints slipped out of place like puzzle pieces that no longer fit.
My little problem.
The neck brace itched, but if I took it off, my head lolled like a marionette’s. The pain was constant now — a deep, grinding pressure behind my skull. I hadn’t worked full-time in over a year. The university let me stay on part-time as a research assistant, but even that felt like running a marathon some days.
I used to dream of earning my Ph.D. Now, I dreamed of sitting up without feeling my spinal cord shift.
Family Pressure
The calls kept coming.
Dad called next.
“Your mother tells me you’re causing trouble.”
“By having surgery?”
“By scheduling it during your sister’s celebration,” he said. “She’s worked hard for this. The least you could do is show up.”
“I could die without this surgery.”
“You always think the worst,” he said. “You’re letting anxiety run your life.”
That word — anxiety — again. The word doctors had thrown at me for years.
Lauren texted that night:
“Typical Casey making everything about your medical drama. You’ve been complaining for years. One more day won’t kill you.”
One more day might actually kill me.
Dr. Henderson’s report had been blunt:
The patient’s cranio-cervical instability is severe. The odontoid process is impinging upon the spinal cord. She is at risk of sudden death from minor head movement.
But apparently, that was less pressing than Lauren’s hors d’oeuvres menu.
Austin
My younger brother was the only one who understood.
“This is insane,” he said one night after family dinner, his voice low and furious. “Dad spent an hour lecturing me about how you’re ‘addicted to playing sick.’ You have actual hardware failure in your spine, Casey. They’re acting like you’ve got a hangnail.”
He squeezed my hand carefully — he’d learned to be gentle after dislocating my fingers once during a hug. “Don’t cancel your surgery. Promise me.”
“I won’t,” I said.
I didn’t tell him that Dr. Henderson’s team had already contacted the New England Journal of Medicine about my case. Apparently, my specific combination of Ehlers-Danlos complications — severe cranio-cervical instability, Chiari malformation, tethered cord — was rare enough to warrant publication. They wanted to document it to help other physicians recognize the signs earlier.
I’d become interesting to science — the kind of patient doctors whispered about in conferences.
Lauren’s Call
A week before surgery, Lauren called. Her tone was pure ice.
“I assume you’re still being stubborn about the party.”
“I’m having life-saving surgery, Lauren. It’s not stubbornness.”
“Whatever. Just so you know, we’re doing family photos at three. Since you won’t be there, we’ll just crop you out of the portrait. Easier than explaining why you chose doctor appointments over supporting me.”
“Doctor appointments?” I repeated, stunned. “Lauren, they’re going to cut through the back of my skull and fuse it to my spine. That’s not optional.”
She laughed — sharp, cruel. “You and your mystery illness. Convenient how you always have some dramatic crisis whenever someone else is getting attention. First, my graduation — you were too dizzy. Then my engagement party — you were too tired. Now my partnership — you need ‘emergency surgery.’”
“I’ve had this scheduled for six months.”
“You could’ve picked another day, but no, you chose my day because you can’t stand anyone else being celebrated. Dad says you’ve got Munchausen’s. That you’re addicted to playing sick.”
The words hit like a blade.
Munchausen’s — the accusation that I was faking everything.
That I wanted to be sick.
Never mind the MRI scans showing my brain stem compression.
Never mind the genetic tests confirming Ehlers-Danlos.
Never mind the fact that every day without fusion risked permanent paralysis.
“I’m sorry I’ll miss your party,” I said quietly. “But I’m having the surgery.”
“Don’t bother coming to the next family event,” she snapped. “We’re all tired of your constant drama.”
Then she hung up.
I cried until the tears triggered a headache so severe I had to lie flat for hours.
Pre-Op Morning
August 12th came.
Austin picked me up at 5 a.m. sharp.
The world outside was gray and quiet. The kind of stillness that feels like a held breath.
“Ready?” he asked.
“As I’ll ever be.”
He tried to make me laugh, joking about how he’d bring a Sharpie to sign my neck ‘Do Not Remove Head’. I smiled weakly. Humor had become our armor.
At the hospital, they checked me in. Pre-op at 6:30, anesthesia consult at 7:00, surgery scheduled for 8:00.
Seven hours, Dr. Henderson had said. Possibly longer.
Austin sat beside me, scrolling through his phone, then frowned. “They really posted photos,” he said.
“Who?”
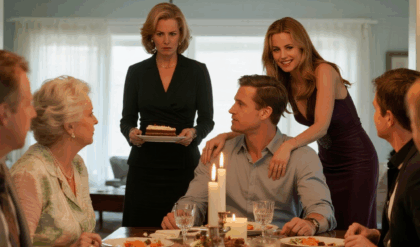
“Mom. Lauren. At the country club. They’re doing family portraits. Right now.”
I closed my eyes. “Of course they are.”
He squeezed my hand. “For what it’s worth, I’m proud of you. For fighting for yourself when no one else would.”
The Surgeons
Dr. Henderson appeared in his scrubs, calm and kind as ever. “Morning, Casey. Ready to get your head back on straight?” he teased gently.
I smiled — his gallows humor was comforting. We’d spent months building trust.
He gestured to the team behind him. “I want to introduce you to a few colleagues observing today. Dr. Patricia Morse from Johns Hopkins, Dr. David Chin from the NIH, and Jennifer Walsh from the New England Journal of Medicine.”
I blinked. “The journal?”
Jennifer smiled warmly. “Your case is extraordinary. We’re documenting the intersection of structural instability and diagnostic failure in Ehlers-Danlos syndrome. With your permission, we’d like to observe the procedure and interview you afterward.”
“Of course,” I said, my voice small. “If it helps others.”
Jennifer nodded. “Your story could change how physicians treat rare disease patients — especially women. You were dismissed for three years, correct?”
“Yes. They said migraines, anxiety, deconditioning.” I touched my neck brace. “One doctor told me to go to therapy.”
Dr. Chin’s face darkened. “This is exactly the pattern we’re trying to fix. Systemic dismissal, delayed intervention. It’s killing people.”
“My family still thinks I’m exaggerating,” I admitted. “They scheduled a party during my surgery.”
A long, heavy silence.
Dr. Henderson’s jaw tightened. “A party?”
“My sister’s promotion celebration.”
Jennifer made a note on her tablet. “Would you consent to including that context? Family invalidation is a critical piece of the narrative.”
“Yes,” I said. “If it helps someone else be believed.”
Into the OR
They wheeled me in at 7:30. The lights were blindingly bright, the air cold and sterile.
I focused on Austin’s voice fading behind me: “You’ve got this, Case.”
And then the world went white.
The surgery lasted nine hours — longer than expected. The instability had been worse than imaging showed. Dr. Henderson later told me they’d had to extend the fusion lower, adding additional hardware.
When I woke, my head felt like concrete — heavy, anchored.
A dull ache, but also relief.
Austin was beside the bed, eyes red. “You made it. Henderson said it was complicated but successful.”
“What time is it?”
“Almost eight p.m. Mom’s been calling. She’s angry.”
I almost laughed. “Why?”
“She said you ruined the family photos.”
Of course I had.
I closed my eyes, exhaustion washing over me. “Let her be angry,” I whispered.
And I drifted back to sleep, the hum of machines steady in my ears.
Part II
The Days After
The ICU never slept.
Machines hummed, monitors blinked, and nurses floated like ghosts through the pale morning light.
Three days after my fusion, I could finally turn my eyes without vomiting. My neck brace wrapped around my skull and jaw, a white plastic halo keeping me alive.
Austin came every day. He’d bring me ice water, talk about random things—baseball scores, campus gossip—anything that wasn’t my spine.
He was twenty-three and suddenly older than everyone else in the family.
On the third morning, Dr. Henderson appeared with his familiar calm smile—and two other people I didn’t know. One wore a Mayo administration badge. The other, a sleek black blazer over hospital scrubs.
“Casey,” Dr. Henderson said, “this is Dr. Susan Morrison, chief of neurosurgery, and Jennifer Walsh from the New England Journal of Medicine. They have something they’d like to share.”
Jennifer lifted her tablet. “Your case study has been fast-tracked for publication. The editors reviewed the preliminary data yesterday. They want it as a lead article.”
My throat went dry. “Already?”
Dr. Morrison nodded. “The severity of your cranio-cervical instability, combined with the years of misdiagnosis, makes it one of the most significant Ehlers-Danlos cases we’ve documented.”
Jennifer smiled. “The ethics board insisted we include commentary on diagnostic delay and family invalidation. We’ll anonymize everyone, of course.”
Family invalidation.
That was one way to describe being told to skip life-saving surgery for a photo session.
Austin squeezed my hand. “You’re going to help a lot of people, Case.”
Later that afternoon, Dr. Morrison returned with imaging on her screen.
“This,” she said, zooming in on the scans, “is what we corrected.”
I stared. Even through morphine haze, it was horrifying—my skull literally sliding forward, the odontoid peg stabbing the spinal cord, the brainstem flattened like soft fruit.
“This,” she said quietly, “is what your family called a ‘little problem.’”
I couldn’t look anymore. “Thank you for believing me,” I whispered.
Dr. Morrison’s expression softened. “Belief shouldn’t be extraordinary in medicine. But sometimes it still is.”
On September 5th, the article went live:
Severe Cranio-Cervical Instability in Ehlers-Danlos Syndrome:
A Case Study of Diagnostic Delay and Family Medical Invalidation
The New England Journal of Medicine.
It featured surgical images, before-and-after scans, and an ethics commentary about the dangers of dismissing rare-disease patients.
Within hours, it hit medical Twitter. By evening, Mayo’s social-media accounts shared it.
By the next morning, it had 100,000 views.
Dr. Henderson called. “Casey, you’re trending in academic medicine. Congratulations—you’re saving lives already.”
The same afternoon, my phone rang again.
Mom’s Call
“Casey,” Mom snapped, “what did you do?”
I closed my laptop. “I had surgery. Like I told you I would.”
“You published an article about us! About how we didn’t support you!”
“It doesn’t name anyone.”
“Everyone knows it’s us!” she shouted. “There can’t be that many daughters who had that ridiculous neck surgery at Mayo in August. Your father’s colleagues are asking questions. Lauren’s firm saw it—her partners are horrified! You’ve humiliated this family.”
I took a slow breath. “You destroyed your own reputation, Mom. I just told the truth.”
“You’re ungrateful,” she said, voice trembling with fury. “We did our best.”
“Your best,” I said softly, “was scheduling a party while I was in an operating room.”
She hung up.
He called an hour later.
“The medical board has the article,” he said without greeting. “Several neurologists think it references my practice. This could affect my license.”
“Then maybe you’ll listen next time a patient says they’re in pain,” I said.
“Don’t be spiteful, Casey.”
“I’m alive because I stopped listening to you,” I said, and ended the call.
Her text arrived that night.
“You’re dead to me.
Hope your precious medical attention was worth losing your family.”
I typed back, then deleted the message before sending:
It was. It saved my life.
Two weeks later, Mayo flew me to the International EDS Conference in Chicago.
I wore a soft brace under my collar and still moved like glass, but I was upright, breathing, alive.
Dr. Henderson presented my imaging to a room of 2,000 physicians.
When he showed the compression of my brainstem, there was an audible gasp.
Then Dr. Morrison took the podium.
“Let’s talk about why it took three years for this patient to be believed,” she said. “Let’s talk about gender bias, rare-disease ignorance, and the role of family dismissal in patient harm.”
When she finished, several people were crying—including me.
Afterward, strangers approached me: a middle-aged woman who whispered, “My daughter has EDS. Her doctors say it’s anxiety.”
A young man who said, “They told me I was crazy too.”
I hugged them all as gently as my fused spine allowed.
For the first time, my suffering felt like it meant something.
Within months, the paper had been cited dozens of times.
Medical schools added it to curricula on rare diseases.
Hospitals updated diagnostic protocols.
Mayo reported a 50 percent increase in referrals for cranio-cervical instability.
Dr. Henderson sent me an email:
“Because of your case, several patients have already been correctly diagnosed. You changed the system from the inside out.”
I printed that email and taped it next to my framed discharge papers.
Mom, Dad, and Lauren sent a joint email:
“You betrayed family trust by allowing publication.
We are deeply hurt and will not be in contact further.”
They told extended family I’d exaggerated everything for attention.
Only Austin stayed.
He moved into an apartment a few blocks from mine, drove me to every follow-up, and clapped like a maniac when my six-month scans showed solid fusion.
We celebrated with cupcakes and bad TV.
“I told you,” he said. “You’re unbreakable now—literally.”
By spring, I was back at the university part-time, researching connective-tissue disorders.
I walked without a brace. I could hold my head high—both medically and metaphorically.
My office wall held two frames:
One for the New England Journal of Medicine article.
One for the family portrait taken at Lauren’s party.
Four people stood smiling before the country-club fountain.
A blank space gaped where a fifth should have been.
That empty space reminded me what survival sometimes costs—and that some absences are necessary.
The medical board quietly opened an inquiry into Dad’s pattern of dismissing patients with neurological symptoms.
Several former patients came forward.
Lauren’s law firm placed her on “extended leave,” citing reputational risk after legal circles discussed the ethics section of my case study.
They might never forgive me.
I’d stopped needing them to.
Because the seventy-three citations, the new diagnostic guidelines, the patients being believed for the first time—those mattered more.
Each day I wake up, I feel the titanium in my neck anchor me to the pillow.
It hums faintly when I stretch—an orchestra of metal and bone reminding me that I chose life.
Sometimes I run my fingers along the thin scar at my hairline and whisper,
“I’m still here.”
And that’s enough.
Part III
Six months after the fusion, I could finally sit up without the world spinning.
I still moved like porcelain, but I could shower without help, cook scrambled eggs, and drive short distances with a brace.
Every morning before work I passed the frame on my wall — the journal article beside the family photo. The gap where I wasn’t standing had become less painful to look at.
It reminded me that survival doesn’t always come with applause.
At the university, I was back in the genetics lab, part-time. My students called me Dr. Mitchell even though I hadn’t finished my doctorate. I corrected them at first, then stopped. I liked the sound of a title earned by persistence, not paper.
Dr. Henderson emailed often, forwarding questions from other physicians:
“Can you clarify how you described the head pressure?”
“Would you speak to a class of residents about early EDS signs?”
I said yes to everything.
The First Talk
My first presentation was at a small teaching hospital in Minnesota.
I wore a dark blazer to hide the brace straps and held the clicker like it was a detonator.
Slide 1 showed my imaging. Gasps rippled through the room.
Slide 2 showed the line from my case study:
Family invalidation and systemic dismissal contributed directly to diagnostic delay.
I told them about the three years of being told to “relax.” About the country-club invitation. About choosing bolts and bone grafts over family photos.
When I finished, a young resident raised his hand.
“How did you stay calm when no one believed you?”
“I didn’t,” I said. “I fell apart. Then I decided falling apart still counts as fighting.”
The room went quiet. Then they clapped — not the polite kind doctors give one another, but the relieved kind that says we needed to hear this.
That evening my inbox flooded.
Patients wrote from everywhere — Iowa, Canada, New Zealand.
“Your article convinced my neurologist to order imaging.”
“They found my instability. I’m scheduled for fusion next month.”
“You saved my daughter.”
I cried reading them.
Every message felt like proof that the suffering had been currency, exchanged for change.
Austin saw me staring at my laptop, tears blurring the screen.
“Good tears?” he asked.
“The best kind,” I said.
Months passed. I half-expected my parents to call eventually — maybe a truce, a grudging acknowledgment.
But the silence stayed.
Birthdays came and went. Christmas arrived with a single card from Grandma addressed only to me and Austin.
Lauren’s firm removed her photo from their website. A contact at the state bar told me she’d taken a “career sabbatical.” I didn’t gloat. I just felt tired.
I realized forgiveness is easier when you stop waiting for it.
By the second year after surgery, hospitals invited me regularly. I wasn’t paid — I didn’t ask to be — but they covered travel and called it “patient-advocate lectures.”
At one conference a rheumatologist said, “You realize you’ve become a case-study celebrity?”
I laughed. “If being famous for neck screws saves one kid from dying misdiagnosed, I’ll take it.”
Dr. Henderson joined me onstage at a national genetics symposium. He called me “the reason half this room started ordering upright MRIs.”
When the applause hit, I looked up at the lights, thinking of the night I lay in a hospital bed while my family posed for pictures.
This applause was louder. And cleaner.
A year later, Austin convinced me to drive past the country club.
The white marble building glowed in the afternoon sun. He parked by the gate.
“You sure about this?” he asked.
“Yeah. I want to see it once and be done.”
A new banner hung outside: Mitchell & Hayes Charity Golf Tournament for Medical Research.
Lauren’s firm again. She was back.
I felt a strange calm. “Good for her,” I said. “Maybe she finally found something worth celebrating.”
Austin glanced at me. “You don’t want to go in?”
“I’ve already been cut open once for that family. Once is enough.”
We drove away. The air smelled like summer rain, and for the first time in years I didn’t flinch when I turned my head.
That fall, one of my genetics students, a shy pre-med named Carla, lingered after class.
“My mom has EDS,” she said softly. “Doctors keep saying she’s anxious. Your article — it’s the only reason I know what’s happening.”
I gave her a copy of my slides and wrote my email on the back.
“Keep pushing,” I said. “For her, and for the patients you’ll have someday.”
She nodded, tears shining. “You make it sound possible.”
“It is,” I said. “Hard. But possible.”
When Mayo Clinic invited me to keynote at their annual neurosurgery symposium, I hesitated. Returning felt like reopening an incision.
But I went.
In the same auditorium where my imaging had once flashed on screens, I stood beside Dr. Morrison.
“This time,” she told the crowd, “our patient is our teacher.”
We discussed updates to the EDS protocol: earlier screening, multidisciplinary teams, mandatory bias training. My case had forced every major teaching hospital to rewrite at least one policy.
Afterward, Dr. Morrison pulled me aside.
“You know, Casey, sometimes progress comes wrapped in pain.”
I smiled. “I’ve got plenty of wrapping paper.”
One night two years post-surgery, my phone buzzed with a number I didn’t recognize.
It was Lauren.
Her voice trembled. “I’m calling because Mom has been sick. She wanted to reach out but didn’t know how.”
Silence.
“She said you’d hang up.”
I didn’t. I just listened.
“I read the article,” Lauren continued. “All of it. I didn’t want to believe it was that bad. I was awful to you.”
“Yes,” I said, because denial helps no one.
“I’m not asking forgiveness. I just wanted to say… I’m sorry.”
The line stayed quiet except for our breathing.
“Thank you for saying it,” I finally answered. “That’s enough.”
When we hung up, I realized I wasn’t angry anymore. Just relieved.
The following spring, the university threw a reception for medical researchers who’d contributed to national policy changes. My mentor insisted I attend.
They handed me a plaque:
For transforming personal adversity into systemic reform.
The applause blurred around me. I could almost hear Mom saying don’t make a scene, but I smiled anyway.
Afterward, Austin raised his glass. “To the sister who kept her head on straight.”
We laughed until it hurt.
That summer, a new paper appeared in the Journal of Neurosurgical Education titled
Integrating Patient Narratives into Medical Curriculum: The Hayes-Mitchell Protocol.
My case had become a verb. To Mitchell meant to document patient experience alongside imaging.
Dr. Henderson sent a note:
“It’s official. You’re part of medical language now.”
I printed it and pinned it next to the photo from the country club. The empty space no longer felt like loss — more like a doorway.
I started a foundation with Austin: The In-Between Project, named for the space between diagnosis and belief. We funded travel for rare-disease patients to reach specialists.
On our website, the tagline read:
“Believe first. Diagnose second.”
Within months, donors from around the country contributed. Some attached notes:
“Because of Casey’s story.”
“Because I was her once.”
“Because belief saved me.”
Three years after surgery, a handwritten envelope arrived — my mother’s careful cursive.
Casey,
I saw your interview on the news about patient advocacy. You looked strong. We were wrong to doubt you. I don’t know how to fix the past, but I want you to know I’m proud you survived.
Love, Mom.
I sat with it a long time before folding it back into the envelope.
Maybe pride was her version of apology. Maybe that was enough.
Now, when I walk across campus in the morning, the titanium in my neck hums gently like a tuning fork.
Students rush past with coffee cups and ambitions, and I remember the woman who once lay flat in bed, praying not to die from turning her head.
At my office door, I keep a small sign:
You are not dramatic. You are data waiting to be believed.
The next part of this story brings Casey to a national stage — an unexpected television interview, a public clash with a skeptical politician, and the moment she finally chooses peace over proving herself.
Part IV
Three and a half years after surgery, a producer from NBC Health Now called my office.
“We’re doing a segment on patient-driven medical reform,” she said.
“Your story changed national protocols. Would you be willing to appear on air?”
I hesitated. I’d spent years learning to live without needing anyone’s validation.
But then I thought of every patient who still sat in a doctor’s office being told it was anxiety.
“Yes,” I said. “I’ll do it.”
The studio was freezing and smelled like hairspray.
A makeup artist clipped my microphone to my collar.
Across the set, the anchor rehearsed my name with practiced sympathy.
“Joining us today is Casey Mitchell, whose experience at Mayo Clinic changed how doctors diagnose rare connective-tissue disorders.”
I took a breath and smiled at the camera’s red light.
She started easy: When did you know something was wrong?
Then: What was it like being dismissed?
I answered calmly until she asked, “And your family? Have things improved?”
There it was. The wound that never quite scarred.
I said, “We don’t speak often. But I’ve learned that family can be anyone who shows up when you’re fighting for your life.”
It aired that night. The clip hit two million views by morning.
Half the comments were support.
The other half called me dramatic, attention-seeking, or “the girl who sued her family” — even though I hadn’t sued anyone.
That’s when I learned fame doesn’t heal old bruises. It just shines a light on them.
Two months later, I was invited to testify before a congressional health-care committee on the importance of early rare-disease diagnosis.
The marble hearing room felt like a cathedral. Reporters whispered. Cameras flashed.
A congressman from Texas leaned forward, skeptical. “Ms. Mitchell, do you really believe bias plays that large a role? Doctors are trained professionals.”
I met his gaze. “Trained doesn’t mean immune to bias, sir. I’m alive because one surgeon chose to listen after dozens didn’t.”
He frowned. “But do you expect taxpayers to fund every patient’s hunch?”
“No,” I said. “Just their right to be heard before they die from one.”
The room went still. Even the stenographer paused.
When I left the Capitol steps afterward, a group of young women waited.
One handed me a folded note: My sister’s doctor dismissed her too. She’s getting a second opinion because of you.
I tucked it into my wallet next to my hospital ID band.
The following week, an opinion columnist wrote:
“Casey Mitchell is brave, but she represents the danger of social-media medicine. Not every patient is a prophet.”
For two days, my inbox filled with hate.
Attention junkie.
Professional victim.
I stopped checking messages until Austin sent a screenshot from a medical forum:
doctors defending me, linking the data, citing the article.
“Let them talk,” he texted. “The work’s speaking louder.”
That winter, Mom called again. Her voice sounded older, thinner.
“I saw you on TV,” she said quietly. “You looked… healthy.”
“I am,” I answered.
A pause. “Your father’s retired. Lauren’s back at work. We— we read about your foundation. You’re doing good things.”
For once, there was no accusation, no demand. Just an awkward bridge over years of silence.
“Thank you,” I said. “I hope you’re all well.”
“We are. And, Casey… I’m sorry we didn’t understand sooner.”
It wasn’t forgiveness, but it was oxygen.
By year five, The In-Between Project had volunteers in twelve states.
We partnered with medical schools, distributing a pocket guide titled
“When the Symptoms Don’t Fit.”
One night after a training session, a young ER doctor approached me.
“I lost a patient once,” he said, eyes wet. “Her scan looked just like yours. I didn’t recognize it. Now I will. Thank you.”
I drove home in silence, the highway lights blurring.
Every mile felt like reclaiming the years I’d spent waiting for someone to believe me.
The email came on a Friday.
Subject: Need legal advice (weird, right?)
Hey Case, I’m representing a client with a rare-disease discrimination case.
I thought of you. Could we talk?
— L.*
I stared at it a long time.
Then I typed back:
Sure. Saturday, noon. Coffee?
When we met, she looked smaller, humbler. She apologized again, sincerely this time.
“I used to think sickness was weakness,” she said. “Now I see it’s survival.”
We talked for hours—about work, about Austin, even about Dad’s garden.
When she left, she hugged me carefully, mindful of the hardware in my neck.
For the first time, it didn’t hurt.
A year later, I stood on stage at the National Patient Safety Awards ceremony, accepting a plaque for “Outstanding Contribution to Diagnostic Reform.”
The emcee mispronounced Ehlers-Danlos twice. I corrected him gently. The audience laughed.
Afterward, a journalist asked, “What does this award mean to you?”
I thought of the invitation on gold-foil linen, of the family portrait without me.
“It means I was right to choose the operating table over the country-club buffet,” I said.
She blinked, unsure if I was joking. I wasn’t.
Carla—the student whose mother had EDS—graduated medical school that spring.
She sent me a photo: white coat, badge, smile.
You told me to keep fighting. I’m a doctor now. Mom’s stable.
We believe because you believed first.
I printed the photo and hung it beside my own surgical imaging.
Proof that stories can heal across years.
August 12th — the sixth anniversary of my fusion.
Austin and I drove to Rochester to leave flowers at the hospital courtyard.
Dr. Henderson met us there, older, silver-haired, still kind.
He shook my hand. “How’s the hardware holding?”
“Solid as ever.”
He smiled. “You’ve done more with your fusion than most do with freedom.”
We laughed, and I realized I could finally tilt my head back far enough to see the sky.
At home that night, I lit a candle and opened the old album Lauren had mailed after we reconciled.
Inside, between baby pictures and report cards, was the country-club photo — now edited.
A recent copy showed a new family shot: Mom, Dad, Lauren, Austin, and me.
They’d taken it the year before, left an open space on purpose.
Under it, Lauren had written in neat script: This time, we waited for you.
I closed the album, tears slipping down my cheeks — not from pain, but release.
That fall, the New England Journal of Medicine published a five-year follow-up titled
“From Case Study to Catalyst: The Mitchell Impact on Rare-Disease Education.”
It listed statistics I already knew: diagnostic times halved, survival rates improved, thousands of physicians trained.
But what caught me was the closing line:
Sometimes one patient’s refusal to be invisible changes how the world sees everyone.
I printed it, framed it, and hung it above my desk.
A decade after the party that divided us, the Stonemont Country Club hosted a charity gala—fundraiser for rare-disease research.
Lauren organized it.
Mom chaired the donors’ table.
Dad spoke briefly about humility in medicine.
When they handed me the microphone, the room hushed.
“I used to think survival meant being believed,” I said. “Now I know it means believing yourself first.”
They stood. They clapped.
Even Mom cried.
Afterward, I stepped outside into the warm night air. The same fountain shimmered under the lights. I touched the edge of my neck brace and whispered, “We made it.”
Years later, when journalists asked why I kept telling the story, I always said the same thing:
“Because somewhere, someone’s mother still thinks her daughter’s pain is a phase.
And until that changes, I’ll keep talking.”
I no longer chase apologies or headlines.
My days are filled with teaching, writing, living.
I plant herbs on my balcony and watch the sun rise without a brace.
Sometimes Austin visits, and we drink coffee under the morning light.
He still jokes, “You sure know how to hold your head high.”
And I do.
Because for the first time, I don’t have to prove I’m alive — I just get to be.
Part V
Ten Years Later
Ten years since the gold-foil invitation.
The envelope still lives in a small box on my bookshelf beside hospital wristbands and a bent titanium screw Dr. Henderson gave me as a keepsake after my one-year scan. “Souvenir,” he’d said with a wink.
Sometimes I take it out and roll it between my fingers.
Cold, solid, permanent — everything my family once thought I wasn’t.
I’m forty now. My neck scars have faded to silver threads.
I can sleep without a brace, run short distances, lift my nephew — Lauren’s boy — without fear of dislocation.
I live in a small house near Lake Superior, where the air smells like pine and the water keeps its own time. My foundation runs itself now. Austin’s the director; I focus on research and writing.
When the wind’s strong, I can almost hear the old voice of my spine creaking, the ghost of instability, whispering, remember.
And I do. Every day. Because remembering is how I honor the girl who refused to reschedule her surgery.
My classroom walls are covered in bright sticky notes left by students and patients:
“Belief saved me.”
“Thank you for teaching empathy.”
“We’re diagnosing EDS earlier because of your work.”
Some nights I stay late grading papers, watching their handwriting blur through tears. The room hums with quiet gratitude, invisible but heavy as gravity.
At the start of every semester, I tell them,
“Statistics matter, but stories change practice. Don’t forget the person behind the chart.”
They listen. They write it down.
That’s when I know the work will outlive me.
The Visit
One snowy afternoon, Mom and Dad showed up unannounced.
I opened the door, startled. They both looked smaller, aged — time and guilt carving them down to gentler shapes.
Mom held a Tupperware of lemon bars, my childhood favorite.
Dad looked at the floor. “We were driving back from visiting Lauren. Thought we’d stop.”
We sat in awkward silence at the kitchen table until Mom said softly,
“You were right.”
I didn’t ask about what. We both knew.
She touched the base of my neck brace. “Does it still hurt?”
“Not like it used to,” I said.
She nodded. “I’m glad.”
Dad cleared his throat. “You’ve done good work, Casey. More than I ever did in forty years of medicine.”
It wasn’t an apology, not exactly, but something close. A truce.
For the first time in a decade, I didn’t feel the need to defend myself.
We ate lemon bars and talked about nothing important.
When they left, Mom hugged me tight — careful but real.
At the doorway she said, “Next time you’re in town, bring that doctor of yours. We owe him a thank-you.”
I smiled. “He’d like that.”
The following summer, Austin got married at a small botanical garden overlooking the lake.
Lauren stood as best man. I was maid of honor.
Mom cried through the vows, Dad handed tissues like confetti.
During the reception, Lauren raised her glass.
“To my sister,” she said, “who taught us all what courage really looks like.”
Everyone clapped. The sound rolled through the garden like forgiveness.
Afterward, we posed for photos.
Five people this time — no empty space between us.
The photographer said, “Hold still,” and for once, I could.
Two weeks after the wedding, an email from Dr. Henderson arrived:
Casey, we’re naming a new patient-education wing. The donors want to call it the Hayes-Mitchell Center for Diagnostic Integrity. Would you consent?
I stared at the screen, heart pounding. The same halls where I’d once been wheeled half-conscious would now carry my name.
I wrote back:
Yes. But make the letters small. The patients’ names should be bigger.
He replied with a smile emoji. I printed the email and pinned it beside the screw on my shelf.
A few years later, a filmmaker from California approached me about a documentary:
“The Girl Whose Family Didn’t Believe Her.”
I refused the title immediately.
“Make it about the system, not my family,” I said.
She agreed.
When it premiered at the Tribeca Film Festival, I flew to New York with Austin and Lauren.
During the credits, old photos of the hospital flashed across the screen — my scans, my brace, my face pale and determined.
The audience stood. Applauded.
Not for tragedy, but for truth.
Backstage, Lauren hugged me, whispering, “You gave me a sister back.”
I whispered back, “You gave me forgiveness.”
The foundation’s mailbox overflows every month — handwritten envelopes from around the world.
One from a teenager in Kentucky:
“They said it was anxiety, but I showed them your article. I’m getting the right care now.”
Another from a retired nurse:
“You taught me to listen again.”
One from a doctor who once dismissed a patient like me:
“I see your face every time I start to doubt someone. Thank you for haunting me.”
I keep them all in a wooden chest under my bed.
My quiet monument.
Five years later, Mayo invited me to deliver the keynote at their centennial celebration.
Standing at that podium, I looked over the sea of white coats and remembered lying on their operating table, my body opened like a question only they could answer.
I told them,
“The real miracle wasn’t the hardware. It was that someone finally listened.
And once you’re heard, you owe it to the next patient to keep the conversation going.”
When I finished, the audience rose.
Among them, Dr. Henderson, older but proud, wiping his eyes.
I spend my evenings watching sunsets over Lake Superior.
The light bends across the water like it’s fusing sky to earth — a different kind of surgery.
Sometimes Lauren visits with her son, now ten. He calls me Aunt Case and asks about the “metal in my neck.”
I tell him it’s superhero armor, and he grins.
In his eyes, I’m not the sick sister. I’m the strong one.
That’s how I want to be remembered — not for the brace or the article, but for surviving long enough to become ordinary.
I keep a journal still — habit from the hospital days.
On the anniversary of my surgery, I wrote this:
Dear Casey (age 26),
You were right to choose the operating room over the party. You were right to believe pain isn’t weakness. You were right that love shouldn’t require pretending you’re fine.
They’ll call you dramatic. Then they’ll call you brave. You’ll outlive both labels.
You’ll teach doctors how to listen. You’ll hold your head high because it’s finally safe to.
Keep fighting.
You’ll make it home.
I folded the page and slipped it between the framed article and the country-club photo.
Ten years to the day after my surgery, Stonemont Country Club hosted another event — not for a promotion, but for a charity fundraiser benefiting rare-disease research.
Lauren sent the invitation. Same gold foil, same elegant script.
Only this time, the date didn’t make me flinch.
When I arrived, the staff greeted me like a guest of honor.
Inside, the ballroom gleamed with crystal chandeliers. A banner read:
“Celebrating Courage: The Casey Mitchell Fund.”
Lauren introduced me from the stage.
“She once lay in an ICU bed while we posed for photos. Tonight, we take a new picture — one that finally includes her.”
Applause thundered.
I stepped up, took the microphone, and looked at the crowd — family, doctors, patients, strangers who’d become part of my strange, beautiful second life.
“I used to think survival meant fighting to be believed,” I said. “Now I know it means believing yourself even when no one else does.”
They rose to their feet.
Flashes from cameras lit the room like the first sunrise after a long night.
And when the photographer said, “Say cheese,”
I smiled — because I was exactly where I was meant to be.
At home later, I replaced the old photo in the frame.
Now five figures stood together again, smiling in front of the same fountain.
The gap was gone.
But I kept the original photo, too — the one with the empty space.
Because that empty space saved me.
It reminded me that absence can be a kind of strength.
That saying no, choosing yourself, walking away — those are forms of love too.
The space meant survival.
Before bed, I wrote a final entry in my journal:
If anyone ever reads this: Don’t wait for permission to save your own life.
Families, doctors, strangers — they’ll misunderstand. Let them.
Live anyway. Believe anyway. Keep your head high, even if it takes titanium to hold it there.
And if you ever find yourself choosing between being loved and being alive — choose alive. Love will follow.
I closed the book.
The house was quiet, the lake outside whispering against the rocks.
Somewhere in the distance, a loon called — that long, haunting sound that always made me feel like the world was listening.
I turned off the lamp, touched the scar at the base of my skull, and smiled into the dark.
Alive.
Believed.
Free.
THE END